As a second Trump administration approaches, we’re running out of time to confirm as many federal judges as possible to provide a check on his presidential power and curb his stated policy priorities.
I Run a Reproductive Rights Hotline. The Stories I Hear Shock Me.

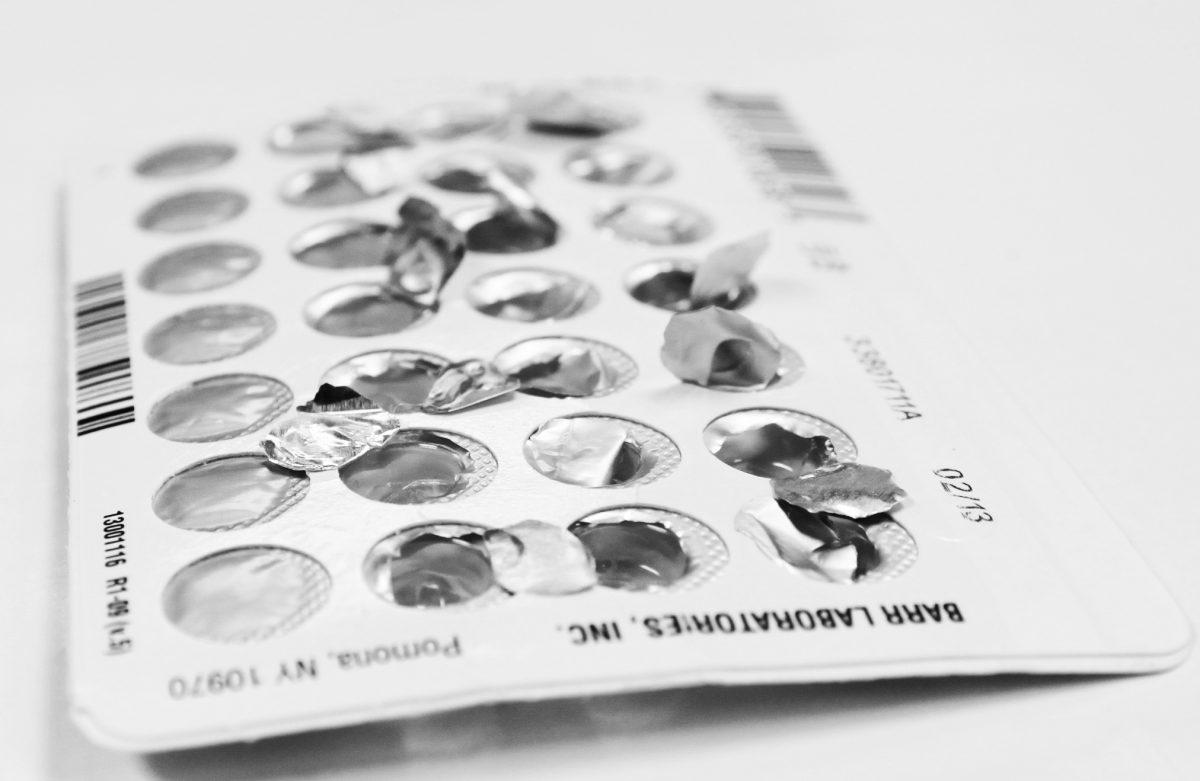
The Affordable Care Act (ACA) requires most private insurance plans to cover contraception—everything from an IUD to sterilization surgery—without any out-of-pocket costs. And yet, there are still too many people who end up with an unexpected medical bill showing up at the door, or in their inbox, weeks or months after accessing care.
Despite guidance – spanning across years – clarifying what the ACA’s birth control benefit covers, I still regularly hear from people whose health plans do not comply with the law. And their stories concern a bunch of different contraceptives:
- Individuals seeking IUDs receive surprise bills for removal, reinsertion, or related services – like ultrasounds prescribed by their doctor – despite federal guidance that requires full coverage of services related to the use and maintenance of birth control.
- People confirm with their insurance plan that it covers their service fully, but later their plan will state that they must meet their deductible before services are covered 100%.
- Plans refusing to cover brand-name drugs like Lo Loestrin FE, claiming that the ACA does not require them to cover every pill on the market. Plans often ignore the requirement that they must cover without out-of-pocket costs the specific pill doctors prescribe due to medical necessity.
The bottom line is… when your health plan does not comply with the law, getting your birth control without any out-of-pocket costs can become a complete mess.
THIS IS NOT HOW THE LAW SHOULD WORK!
Since Dobbs, methods like sterilization surgery have become increasingly popular. In the past few years, Bilateral Salpingectomy – a surgery where both fallopian tubes are removed – has become a new option for sterilization, with the additional benefit of reducing the risk of ovarian cancer. Even so, plans often don’t recognize the billing codes for bilateral salpingectomy as “preventive care,” thus resulting in bills ranging from the hundreds to the thousands.
I could spend days waxing poetic on my soapbox about coverage issues like these (and many others.)
It’s easy to identify when a plan is not complying with the law, but it can be challenging for most people to resolve these coverage issues. One of the best ways to fix coverage is to file an appeal with your plan, which can be a tiring and long process. It’s not uncommon for individuals to spend months trying to get their plans to comply with the ACA. Still, I find that people who keep pushing back against their insurer’s coverage decision experience success. It’s always great to hear when someone faced with a $1000+ bill is now expected to pay $0. As it should be.
All in all, more needs to be done. There is hope that the Biden Administration is finally hearing our pleas to fix the gaps that prevent people from accessing full coverage. Earlier this summer President Biden issued an Executive Order (EO), encouraging the Secretaries of the Treasury, Labor, and Health and Human Services to issue more guidance that would ensure coverage to contraception without out-of-pocket costs.
While I’m encouraged by the Biden’s Administration action, we need MORE than just guidance. Insurance companies have flagrantly violated the ACA for years. The Secretaries should also use their enforcement powers to guarantee that health plans understand the consequences if they fail to cover birth control. Gaps in coverage will persist if issuers are not penalized for ignoring coverage requirements.
As we wait for this change, however, we cannot leave patients in the lurch.
For as long as it takes, CoverHer will continue to support those who need help getting the coverage they deserve.