#WorstTBTEver: When Americans Living with HIV Couldn’t Get Health Insurance Coverage

 The Affordable Care Act (the ACA or “Obamacare”) has improved America’s health across the board, mostly by getting more affordable health coverage to more people and making sure health insurance covers the care people need. For people living with HIV, the ACA has been especially important. But this progress is in jeopardy as Congress moves to repeal the ACA and undo the many protections the law has provided for people living with HIV.
The Affordable Care Act (the ACA or “Obamacare”) has improved America’s health across the board, mostly by getting more affordable health coverage to more people and making sure health insurance covers the care people need. For people living with HIV, the ACA has been especially important. But this progress is in jeopardy as Congress moves to repeal the ACA and undo the many protections the law has provided for people living with HIV.
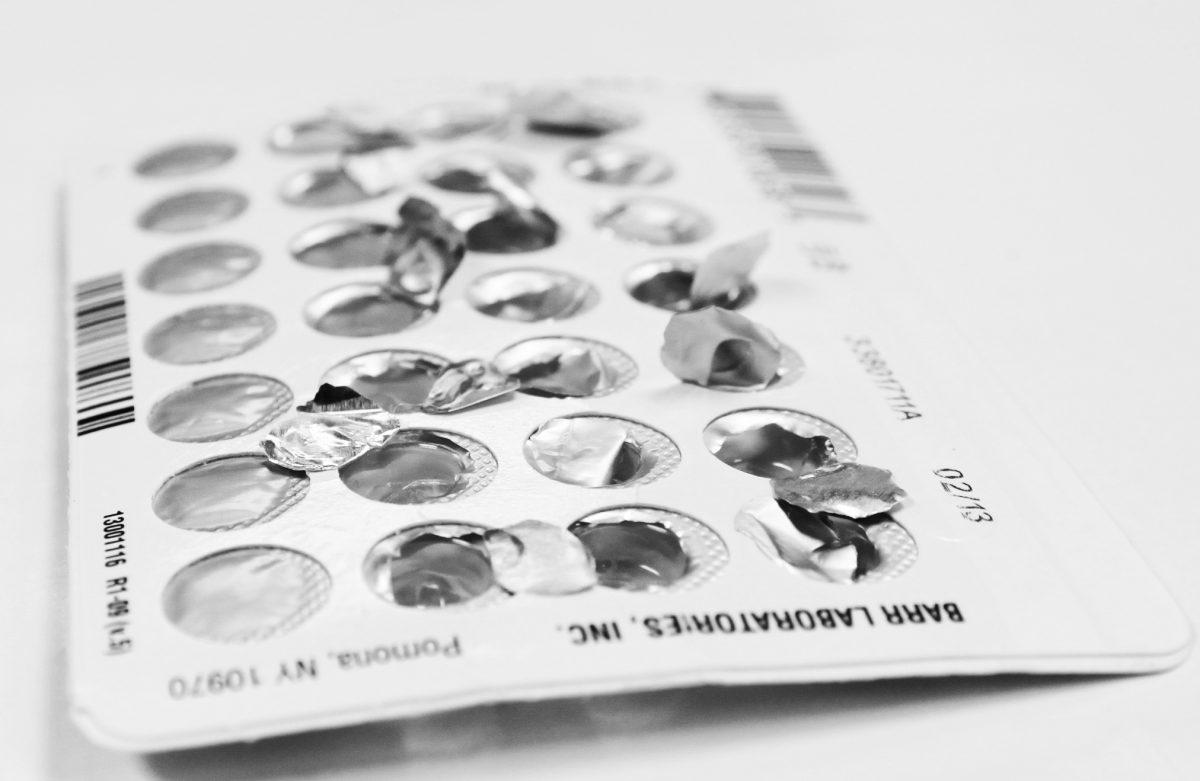
Before the ACA, insurers could deny health coverage based on preexisting conditions, and being HIV positive often meant denied health coverage.
Even if a person living with HIV had insurance coverage, many insurance plans failed to include critical HIV medications on their formularies, despite covering medications for other chronic diseases. Furthermore, limits or caps on coverage meant many of the expensive treatments and medications a person with HIV needed would not be covered, resulting in high out of pocket costs to patients. Now, the protections in the ACA keep plans from denying coverage for preexisting conditions, including HIV. The law also requires plans to include HIV medications on their formularies if they covered other medications and lifts limits on coverage so that insurance plans provide coverage for people when they need their health plan the most.
Thanks to the ACA, the uninsured rate for all Americans is at an all-time low, and new data show that this is especially important for people with chronic conditions like HIV.
New analysis by the Kaiser Family Foundation highlights just how important the ACA has been for people living with HIV, especially in states that expanded Medicaid. The uninsurance rate for people living with HIV in care fell from 13% in 2012 to 7% in 2014 in the Medicaid expansion states sampled in the survey. The analysis also highlights the importance of the ACA for people of color broadly, but especially Black Americans living with HIV. Uninsurance rates among Black individuals with HIV in care dropped from 21% in 2012 to 4% in 2014. This was true in both Medicaid expansion states, where uninsurance dropped from 13% in 2012 to 5% in 2014, and non-expansion states, where uninsurance dropped from 29% in 2012 to 22% in 2014. Still, gains in coverage for Black individuals with HIV in care were most dramatic in states that expanded Medicaid.
Women of color stand to lose the most in terms of access to health coverage and quality health care if the ACA is repealed.
Our own state-by-state analysis of health insurance coverage of women of color from 2013 to 2015 similarly found that women of color accounted for two thirds of the gains made in coverage under the ACA, while they make up only about a third of women with health insurance. Double digit gains in health coverage of women of color in nearly every state were due mainly to expanded Medicaid eligibility (in states that expanded Medicaid) and access to affordable coverage through the health insurance marketplace that were part of the ACA.
Access to stable health coverage and regular care is critical for individuals living with HIV to remain active members of their communities, prevent advancement of the disease, and live health lives.
Access to health coverage and care is also critical for HIV prevention, especially in communities that experience disparities in rates of new HIV infection and that lack access to preventive care and treatment, including Black women. According to CDC, Black women account for 62% of all new HIV infections among women and are more than three times more likely than white women to live with HIV. Black women are less likely to have access to health insurance coverage and are more likely to lack access to regular care because of complex interactions of economic, social, and cultural factors. Disparities are especially acute for Black transgender women. A recent survey of the transgender community found that nearly 1 in 5 Black transgender women is living with HIV, and intersecting barriers, including lack of health coverage, health care costs, and healthcare discrimination impede access to prevention and care.
Repeal of the ACA , or changes to the Medicaid program, ignores how important the law has been in improving the lives of many millions of people in this country, especially those living with chronic conditions such as HIV.
The ACA has been a watershed for health equity. Individuals living with HIV, especially in communities that experience disparities and barriers to care, are uniquely at risk if the ACA is repealed. As demonstrations at town halls across the country show, people are not interested in turning the clock back on progress made thanks to the ACA, especially from the life-saving care many living with HIV now have access to.
Don’t miss our other #WorstTBTEver blogs:
Post 1: When Millions of Women Fell into the Coverage Gap
Post 2: When Being a Woman Was a Pre-Existing Condition
Post 3: When Health Insurance was Out of Reach
Post 4: When Your Zip Code Determined Whether You Could Get Affordable, Comprehensive* Health Insurance
Post 5: When There Was an Unmet Need for Birth Control Coverage
Post 6: When There Were “Winners” and “Losers” in Health Care