As a second Trump administration approaches, we’re running out of time to confirm as many federal judges as possible to provide a check on his presidential power and curb his stated policy priorities.
Racism in Health Care – For Black Women Who Become Pregnant, It’s a Matter of Life and Death

Women in the United States die during or after pregnancy at higher rates than almost anywhere else in the developed world. And unlike most other countries the maternal mortality rate keeps rising. The rates are particularly stark for women of color, and Black women in particular. Black women are three to four times more likely than white women to die from complications during pregnancy or childbirth.
This week is Black Maternal Health Week (April 11th-17th), founded and led by the Black Mammas Matter Alliance. #BMWH18 is drawing attention to the barriers Black women face when attempting to access the pregnancy care they need. But as we, particularly white folks like myself, are asking why this is happening, we cannot ignore what Black folks already know, that racism, including racism in health care, is contributing to the deaths of Black women.

Racism disproportionately effects the quality of care mothers receive during childbirth. For example, research has shown that implicit racial bias may cause doctors to spend less time with Black patients, and that Black people receive less effective care. Providers are also more likely to underestimate the pain of their Black patients, ignore their symptoms, or dismiss their complaints.
Take tennis star Serena Williams for example. The day after giving birth, Serena Williams felt short of breath. Knowing her body and her history of developing blood clots in her lungs she told her health care providers that she was having trouble breathing. They initially ignored her concerns, chalking it up to the medication Williams was on – it was making her confused, they said. Serena Williams was eventually able to insist that her providers give her the care she needed, which saved her life. But for many Black women, when a provider’s initial reaction isn’t to take their pain or symptoms seriously, they don’t get the care they need.
Serena Williams’ story is not unique. In the more than 200 stories of African-American women collected by NPR and ProPublica, the feeling of being dismissed, devalued, and disrespected by health care providers was a constant theme. For example, one new mother from Nebraska with a history of hypertension couldn’t get her doctors to believe she was having a heart attack until she had another one. Another woman, a Chicago-area businesswoman with a high-risk pregnancy, was so upset at her doctor’s attitude that she changed OB/GYNs in her seventh month, only to suffer a fatal postpartum stroke.
The bias and discrimination Black women face when getting medical care compounds the harm of already existing inequality. For example, although the Affordable Care Act has made important gains in helping to reduce uninsurance rates of women of color, including Black women, disparities still remain. Black women are more likely to be uninsured before they become pregnant, making them more likely to start prenatal care later. Lack of health insurance can also keep Black women from getting the postpartum care they need. Black women are also more likely to have chronic conditions such as obesity, diabetes, and hypertension that make pregnancy more dangerous. Furthermore, the hospitals that serve predominantly Black neighborhoods, where many Black women give birth, provide lower quality care than those where white women deliver.
Black women consistently receive this lower-quality care regardless of age, socioeconomic status, and education. For example, Shalon Irving, an epidemiologist at the Center for Disease Control and Prevention, and a Black woman, died three weeks after giving birth from complications of high blood pressure. Even with two masters degrees, a PhD., health insurance, and a strong support system Shalon Irving still died from pregnancy complications.
When Black women with economic and educational advantages like Shalon Irving continue to die at higher rates than white women it shows that education and access alone won’t solve this problem.
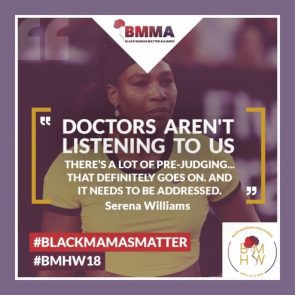
So this week, as we increase attention to the issue of maternal mortality in the United States, we should make the implicit explicit – that there is racism in health care contributing to poor health outcomes for Black mothers and their babies; that providers have and continue to ignore the pain and symptoms of Black women who are pregnant, regardless of how much money they make or how famous they are; and that until we address racism in health care our goal of improving Black maternal health cannot be realized.




